U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation
This study addressed a series of policy questions related to the impact of CHIP, the effective operation of CHIP programs, and the inter-relationship between and among CHIP, Medicaid, and employer-sponsored insurance coverage for low-income children.
The Children's Health Insurance Program Reauthorization Act of 2009 (CHIPRA) 10-State Evaluation of the Children’s Health Insurance Program (CHIP) was a congressionally mandated evaluation to explore how CHIP has evolved since its early years. This study addressed a series of policy questions related to the impact of CHIP, the design and operation of CHIP programs, and the relationship between CHIP, Medicaid, and employer-sponsored insurance coverage for low-income children. It evaluated the impacts of CHIP on children’s coverage and access to care and assessed new issues that have arisen as a result of CHIPRA and the Patient Protection and Affordable Care Act (ACA).
Evidence & Insights From This Project
Research Recap: CHIP Improves Children's Access to Care, Eases Financial Burden on Families
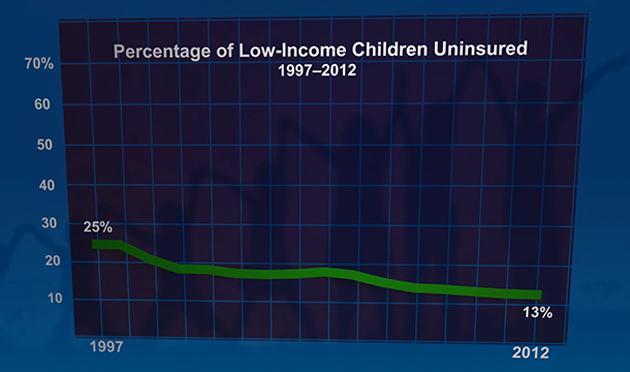
New evidence from a nationwide evaluation of the Children's Health Insurance Program (CHIP) reveals that CHIP has successfully expanded coverage for children who would otherwise be uninsured.
Learn MoreCHIP Improves Children's Access to Care, Eases Financial Burden on Families (In Focus Brief)
Congressionally Mandated Evaluation of the Children's Health Insurance Program: Texas Case Study
Congressionally Mandated Evaluation of the Children's Health Insurance Program: Ohio Case Study
Congressionally Mandated Evaluation of the Children's Health Insurance Program: Michigan Case Study
Related Staff
See Clearly. Act Quickly.
From local to global challenges in health, human services, and international development, we’re here to improve public well-being and make progress together. Learn more about becoming a Mathematica client or partner.
Work With Us





