For the first time in agency history, the Center for Medicaid & CHIP Services (CMCS) can produce estimates of the racial/ethnic distribution of enrollees in Medicaid and the Children’s Health Insurance Program (CHIP) that include all enrollees. This capability provides insights that previously had not been possible due to missing or unusable self-reported data on race/ethnicity.
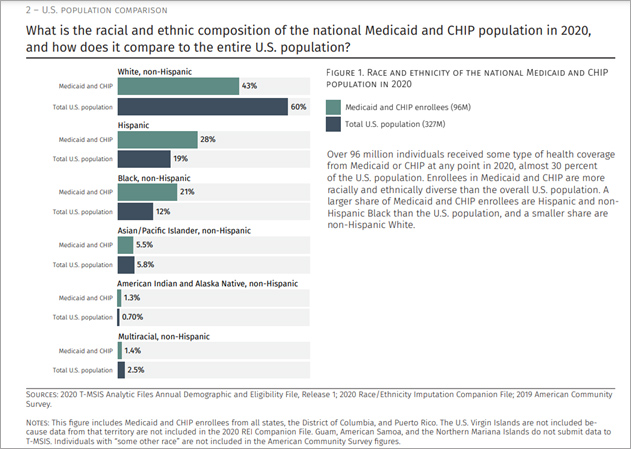
CMCS can now report that of the 96 million enrollees in 2020, there were an estimated 41 million non-Hispanic White Medicaid and CHIP enrollees, 27 million Hispanic enrollees, 20 million non-Hispanic Black enrollees, 5 million non-Hispanic Asian/Pacific Islander enrollees, and 1 million non-Hispanic American Indian and Alaska Native enrollees, with the remaining enrollees being multiracial. Mathematica worked with CMCS to make this analysis possible by developing indirect estimates of enrollees’ race/ethnicity when those data are unavailable or unusable, an effort that CMS recently highlighted in a blog post.
"Better data on race and ethnicity can improve CMCS' ability to understand disparities in access, quality, experience, and outcomes for Medicaid and CHIP enrollees," said Laura Nolan, senior researcher at Mathematica who led the initiative to enhance the race/ethnicity data in CMCS’ Medicaid and CHIP enrollment records. "While states continue to improve their reporting of this information, enhancing the data using statistical methods is important for supporting evidence-based decisions made by the agency. Mathematica collaborated with CMCS to enhance its race and ethnicity data via a well-validated, evidence-based method that combines self-reported data with indirect estimates."
CMCS needs high-quality data to realize its vision of reducing disparities in access, quality, experience, and outcomes in Medicaid and CHIP. To help support this vision, Mathematica has partnered for years with the Data and Systems Group within CMCS, as part of the Medicaid and CHIP Business Information Solution data analytics and data quality project. This work includes supporting states submitting Medicaid and CHIP data, developing research-ready analytic files and analytic products based on these data, along with implementing continuous improvement of the data. However, states continue to have challenges reporting complete and accurate race/ethnicity data, which are missing for about a quarter of Medicaid and CHIP enrollees. The COVID-19 pandemic and the racial/ethnic disparities in both experience of care and outcomes brought new urgency to improving race/ethnicity data for Medicaid and CHIP enrollees.
With these more complete data, CMCS can include all Medicaid and CHIP enrollees when developing analytics by racial/ethnic group for program monitoring, evaluation of policy implementation, and oversight. More complete data can help prevent biased conclusions based on a nonrepresentative subset of enrollees, as well as enable researchers to stratify quality and outcome measures by race/ethnicity to highlight opportunities to close disparities in experience.
This work is part of CMCS’ push toward increased transparency and information about racial and ethnic disparities in Medicaid and CHIP. As part of this strategic vision, CMCS recently published equity data briefs that draw on its work with Mathematica to enhance race/ethnicity data. Of the more than 96 million people covered by Medicaid or CHIP at any point in 2020, a much larger share were in a racial/ethnic group other than non-Hispanic White (57 percent) compared with the general U.S. population (40 percent). This figure below highlights the crucial role that Medicaid and CHIP play in providing health insurance coverage to everyone.
Contact
-
David Roberts
droberts@mathematica-mpr.com
202-270-9439

