New evidence from a nationwide evaluation of the Children's Health Insurance Program (CHIP) reveals that CHIP has successfully expanded coverage for children who would otherwise be uninsured, thereby increasing their access to care and reducing financial burdens on their families. Mandated by the Children's Health Insurance Reauthorization Act (CHIPRA) of 2009, this evaluation presents new information on the evolution of CHIP from 1997 to 2012, including whether the program is meeting its goals and how it was affected by CHIPRA and the Affordable Care Act.
The evaluation revealed that:
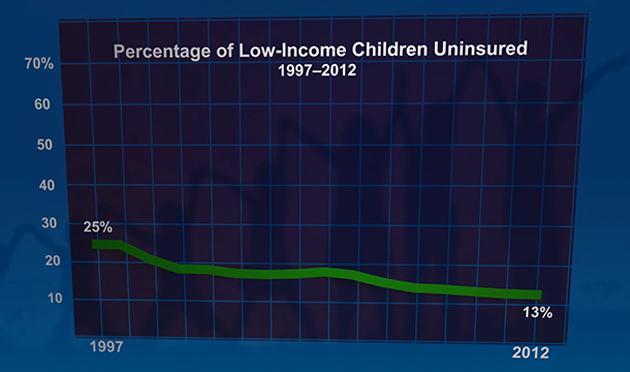
- CHIP, combined with Medicaid, contributed greatly to the decline in uninsured rates among low-income children, which fell from 25 percent in 1997 to 13 percent in 2012.
- Since CHIP was enacted, coverage rates improved for all ethnic and income groups, and coverage disparities narrowed significantly for Hispanic children.
- Children in Medicaid and CHIP had better access to care, fewer unmet needs, and greater financial protection than uninsured children
Implications for the future of CHIP
Findings from this evaluation can inform future decisions about CHIP funding, policies, and programs. The positive impacts of CHIP were found for children and families in states with various program designs and features, across demographic and socioeconomic groups, and for children with a range of health care needs. However, improvements are needed to address remaining unmet needs for care, to reduce the percentage of children who cycle off and back on to Medicaid and CHIP, and to reach the estimated 3.7 million children who are eligible for Medicaid or CHIP but remain uninsured.