
Carol Irvin
Senior Fellow
View Bio PageStronger programs start with stronger data. By modernizing Medicaid’s digital infrastructure, state and federal agencies can generate timely insights that support better decisions and healthier outcomes.

As a result of our work for CMS, the number of states meeting overall data quality targets nearly doubled in just three years.
The Centers for Medicare & Medicaid Services (CMS) requires states and nonstate jurisdictions to submit claims records for everyone enrolled in Medicaid and the Children’s Health Insurance Program (CHIP). Given the scale of those programs, the records can shed light on the effectiveness of federal safety net programs that support the health of more than 78 million beneficiaries.
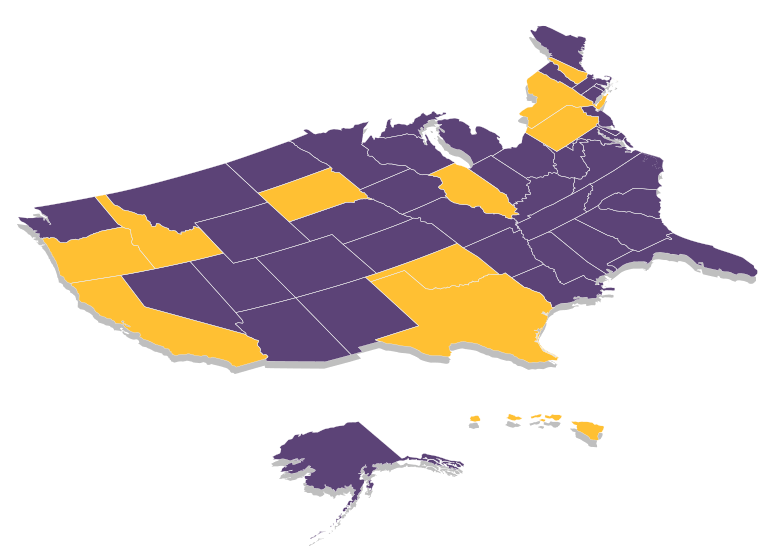
But with 50 states, the District of Columbia, and U.S. territories submitting records to the Transformed Medicaid Statistical Information System (T-MSIS) based on their own systems and methods for collecting data, CMS faces the challenge of standardizing raw data so the data can be analyzed quickly and used to guide research, policy, and program decisions.
Mathematica’s integrated team of policy experts, data scientists, methodologists, and technologists worked with CMS to make states’ raw data more user-friendly for federal and state agency officials, congressional staff, and researchers, ultimately to improve the cost-effectiveness and outcomes of Medicaid and CHIP. Drawing on our expertise with Medicaid and CHIP as programs and as rich sources of data for policy research, we focused on:
By making state Medicaid and CHIP data reliable and analysis ready, we laid the foundation for timely, high-quality solutions to urgent policy questions. For example, at a time of public concern about rising healthcare costs, CMS is using the data to reduce improper spending and strengthen program integrity by addressing duplicative enrollment in Medicaid. By regularly checking and reporting on the quality of states’ Medicaid and CHIP data, we’ve also helped make state records more reliable and complete, improving their usefulness for informing policy and programmatic decisions. As a result of our work for CMS, the number of states meeting overall data quality targets nearly doubled in just three years.
To solve their most pressing challenges, organizations turn to Mathematica for deeply integrated expertise. We bring together subject matter and policy experts, data scientists, methodologists, and technologists who work across topics and sectors to help our partners design, improve, and scale evidence-based solutions.
Work With Us