Funders and think tanks have championed big data, technology, and analytics to improve health in low and middle-income countries (LMICs), spurred on by the promise of applying the principles of precision medicine to global health. However, without addressing rampant foundational problems with data collection, access, and use in LMICs, they are unlikely to reap the full benefits of their investments.
The evidence linking data improvements and better health remains limited, but our Health and Equity Data Framework illustrates how data collection, access, and use could better support health decision making that might advance health equity. It offers changemakers in global health a model to gauge progress on the path to data equity and assess the relationship between data and health. Case studies show the potential social good that better data could help achieve; for example, researchers have used anonymized cell phone data that shows people’s movements to anticipate and respond to disease outbreaks, such as malaria in Senegal. The government of Sierra Leone uses satellite data to map the location of registered community health workers (CHWs) and identify communities that don’t have CHWs, enabling its Ministry of Health to optimize the training and deployment of CHWs.
However, when this data is of low quality, it inevitably leads to less accurate analysis and results. And even high quality data cannot be maximized by LMICs without a workforce and the infrastructure to support it. The lack of these resources partially explains why few LMIC investments in data analytics have borne fruit at scale. Further, there is potential harm in running analytics on poor quality data and perpetuating biases.
To use data effectively to improve health and advance equity in LMICs, we need to go “back to basics” so that insights derived from health data in LMICs reflect reality. This means working toward a state of data equity in which all people have access to high quality data and the capacity to use it effectively to achieve results.
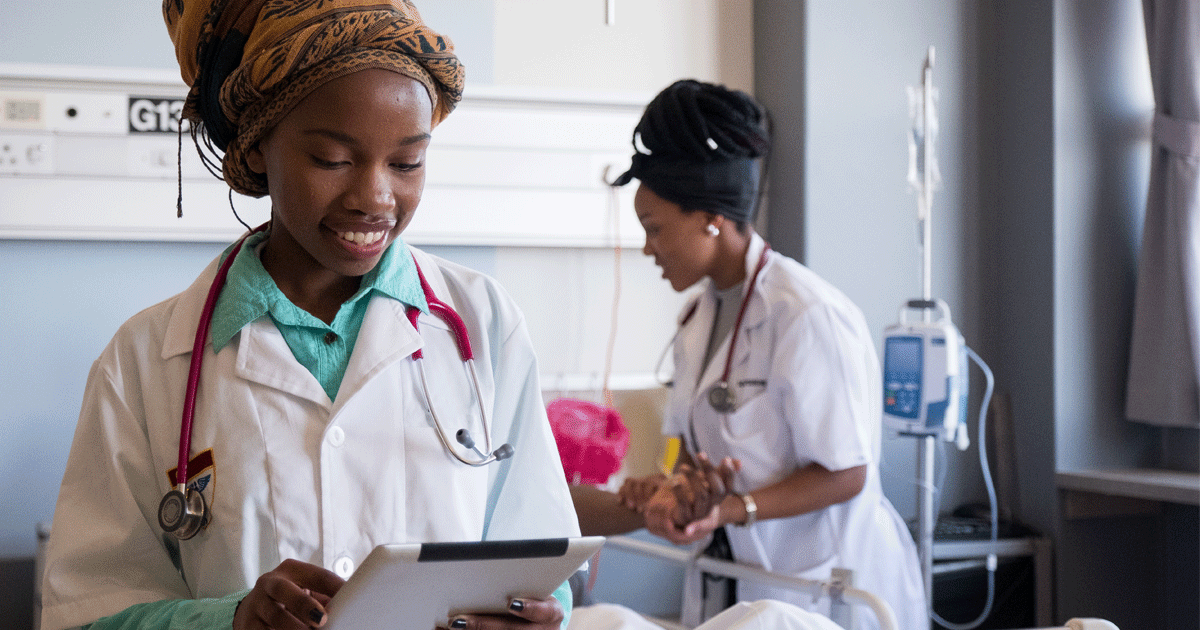
First, achieving this goal requires collecting the data needed to gain insights and inform decision making. Data collection should be efficient, streamlined to reduce burden and duplication, and representative of all populations, especially historically marginalized populations like women, children, and refugees. Data collectors should have regular training and supervision so that the data they collect are of high quality—accurate, standardized, complete, and up-to-date. The World Health Organization has issued guidance on how to improve these dimensions of data quality. Philanthropic, bilateral, and multilateral donors and nongovernment organizations (NGOs) have answered the call, partnering on projects like the Better Immunization Data Initiative to improve data and information for immunization in select LMICs.
Beyond collection, government officials, health systems administrators, and informatics staff can improve data accessibility by making collected data available at all levels of the health system, as well as in sectors outside of health. This will facilitate timely and accurate data-driven decision making. To increase data access, information systems should be interoperable, with data made open by default and published in formats that are conducive to rigorous analysis, such as CSV or XLS files. For example, data that are downloadable and machine-readable with an open data license, rather than a PDF posted on a health ministry’s website, will be more user-friendly and accessible. When data are more accessible, not only are decision makers within the health sector better able to use them for resource allocation, stock management, budgeting, policy planning, and so on—but researchers outside of the contexts in which the data were initially collected are able to use them for novel applications. It is important to note, though, that the surrounding policy environment should encourage data sharing while protecting privacy and security by building the necessary legal frameworks and oversight bodies to do so. NGOs in the open data movement have developed specific calls to action for years to stimulate global progress in improving data access. COVID-19 has highlighted the inadequacies in current data collection and access and the urgency of answering this call.
Finally, to fully unleash the power of data, funders and government officials within LMICs need to make data easier to use. For example, they should provide affordable broadband internet access, bolster computer literacy skills across the education system, and develop learning hubs to make advanced data science training and education available across the Global South. In addition, stewards of the data and those conducting analyses should prioritize its interpretation with community members to demonstrate how it can benefit the community from which it was collected and can promote data use in the localities from which it came. Community engagement with the data could come through data placemats and data walks in which those collecting and analyzing the data develop materials to facilitate community discussion and interpretation of the data. This, in addition to training on routine analytics for health workers and health decision makers, could help foster a stronger culture of demand for data to generate insights for decision making.
Getting back to the basics of improving how data is collected, accessed, and used is the first significant step in improving the accuracy of many big data innovations in LMICs. Big data, technology, and analytics hold great promise to help ensure global health equity, but foundational issues with data need to be addressed first to determine whether improved data can help achieve this goal.